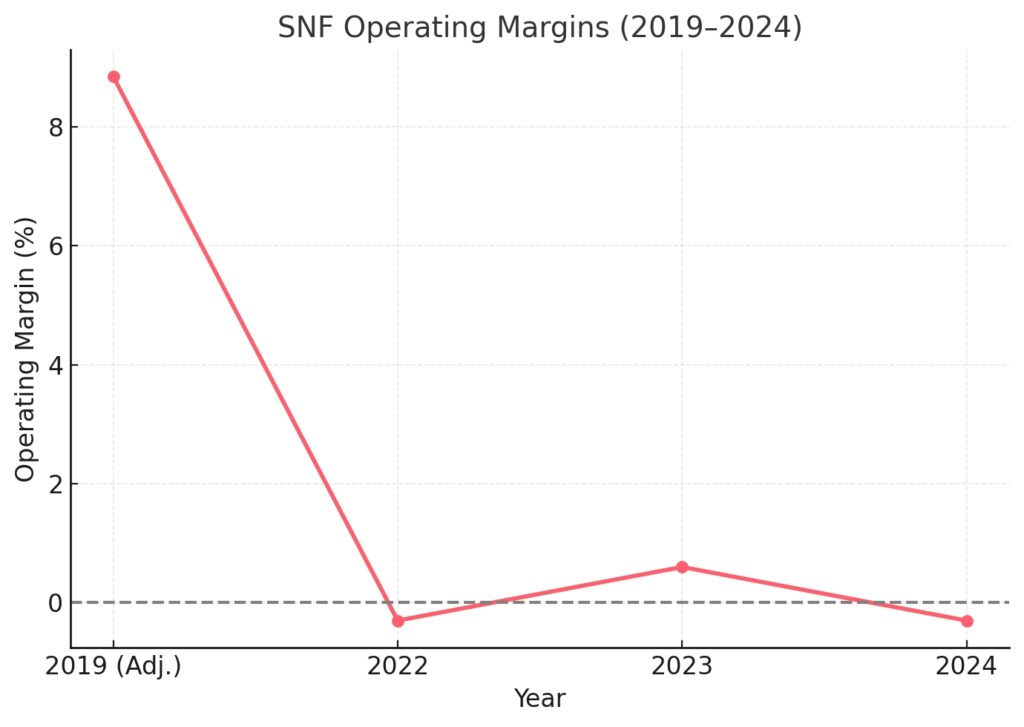
If you run a nursing home, you don’t need me to tell you that margins are painfully thin—you feel it every day. Some weeks it’s like juggling three things at once: payroll climbing higher, reimbursements that never quite cover the cost of care, and regulators who always seem to be adding new rules. All of that, while you’re still expected to deliver quality care around the clock And the numbers back it up. The median skilled nursing facility operating margin was about -0.3% in 2022, and by 2024, nearly 45% of facilities said they were operating at a loss. That paints a grim picture. But here’s the thing—some nursing homes are not just getting by, they’re actually thriving. That gap isn’t about luck. It’s about the way they run their operations.
One of the biggest misconceptions in our fi eld is that the only way to “save money” is to cut staff or lower care standards. That couldn’t be further from the truth. In fact, the most successful operators are proving the opposite: profitability comes from smarter processes, stronger teams, and sharper fi nancial discipline—not from cutting corners on care.
That’s exactly what this blog is about. I’ll walk you through five practical, data-backed ways nursing home owners can improve profit margins without cutting care quality. These are strategies you can take back to your facility today, and they’ll work whether you’re a small operator or running a multi-facility group.
1. Boost Occupancy & Admissions Efficiency
Every empty bed in your facility is lost revenue. With labor, utilities, and compliance costs rising, you can’t afford to let beds sit unfi lled. Yet across the U.S., many nursing homes face exactly that challenge—not because there isn’t demand, but because operational bottlenecks are holding them back.
The good news? Demand is strong. Skilled nursing facility occupancy rebounded to 84% in October 2024, up from the pandemic low of 67%. That’s a huge recovery. But here’s the catch: between 46% and 61% of facilities still limit new admissions because they don’t have enough staff to safely care for residents. In other words, the demand is there, but many providers can’t capture it.
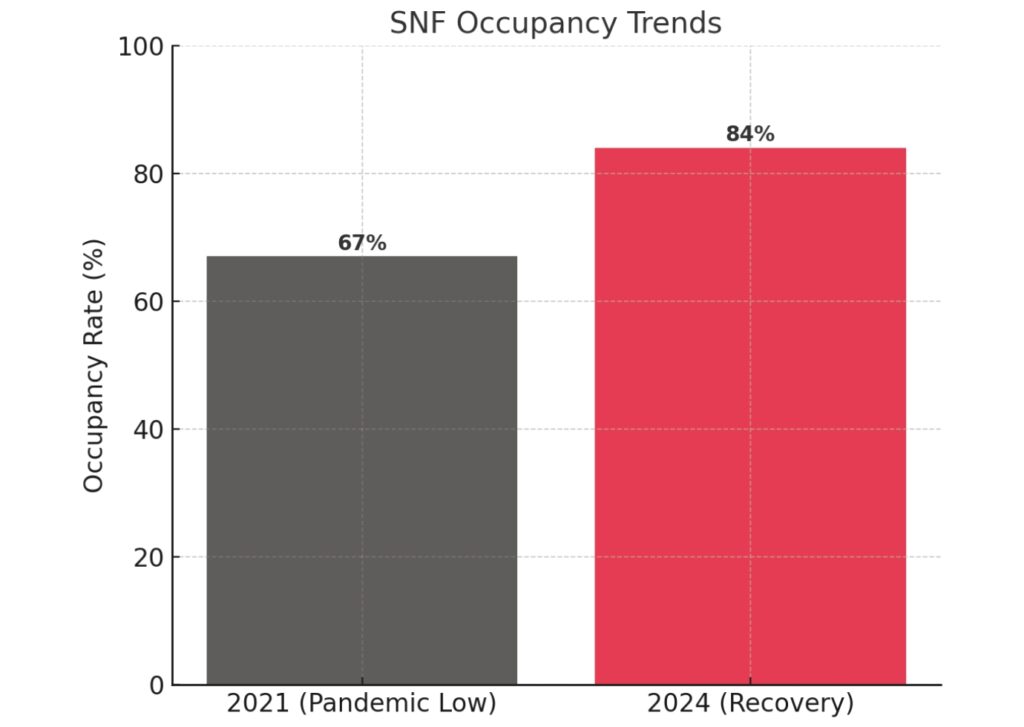
Financially, even small occupancy gains are powerful. A 1% increase in census at a 100-bed facility can generate ~$146,000 in annual revenue. The real margin booster comes from payer mix: one Medicare FFS resident brings in $587 per patient day, compared to $270 for Medicaid. Medicare Advantage prior authorizations can delay discharges by 72 hours or more. Every day lost in paperwork is revenue deferred, and in some cases, revenue lost forever.
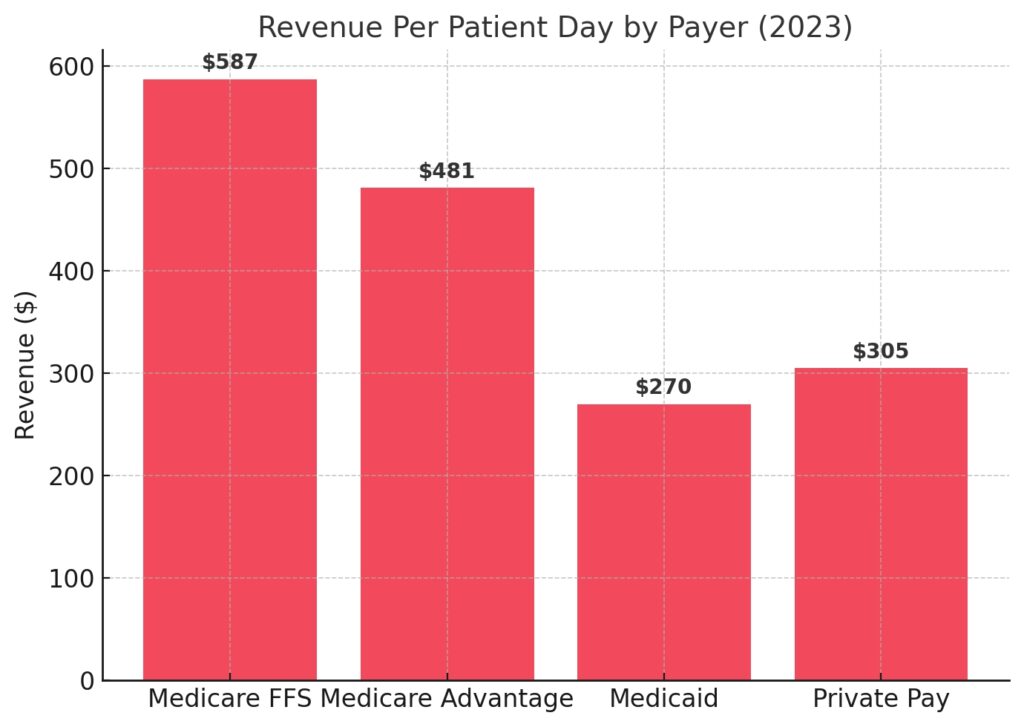
The takeaway is simple: improving your admissions and eligibility verifi cation process is one of the fastest ways to improve margins—without cutting care. By reducing administrative drag and strengthening hospital referral relationships, you can boost occupancy, shorten turnaround time, and capture the residents who bring the highest reimbursement.
2. Reduce Waste & Capture All Earned Revenue
Here’s a hard truth: most nursing homes lose money they’ve already earned. Not because the care wasn’t provided, but because of administrative errors, billing issues, and supply chain waste. These hidden leaks quietly eat away at margins every single day.
Take claims, for example. In 2023, 14.9% of Medicare Part A claims for SNF services were improper, representing $4.8 billion in lost revenue across the sector. Even more telling—79% of these denials were due to insufficient documentation, not medical necessity. That means facilities are providing the right care but failing to capture payment because of missing or incorrect paperwork. It’s like working for free. The same story plays out in supply chains. Hospitals waste an estimated $25 billion each year on inefficient supply management, and SNFs—often with smaller budgets and fewer controls—mirror that waste on a proportional scale. Overstocked supplies expire on the shelf. Understocking forces emergency orders at premium prices. Simple mistakes in waste segregation (like throwing general trash into costly regulated medical waste bins) drain budgets unnecessarily.
For a facility operating on margins as slim as 1–2%, this kind of leakage can mean the difference between profi t and loss.
The solution isn’t to cut care—it’s to tighten processes. Facilities that invest in billing automation, clinical documentation improvement, and smarter inventory management protect revenue that’s already earned. Every denied claim successfully overturned, every supply dollar spent wisely, drops straight to the bottom line.
3. Invest in Workforce Retention & Smarter Scheduling
If you want to understand where your money is going, look at your payroll. Labor makes up two-thirds of nursing home revenue, and when turnover runs high, the fi nancial bleeding gets even worse.
The data is staggering. In 2024, overall nursing staff turnover in nursing homes was 48.7%, with CNAs at 63% and RNs at 50%. Replacing a single RN costs about $56,300, while CNA replacements run $3,000–$6,000 each. For a typical 100-bed facility, turnover can cost ~$594,000 annually—money that could have been reinvested in staff wages, facility improvements, or resident care.
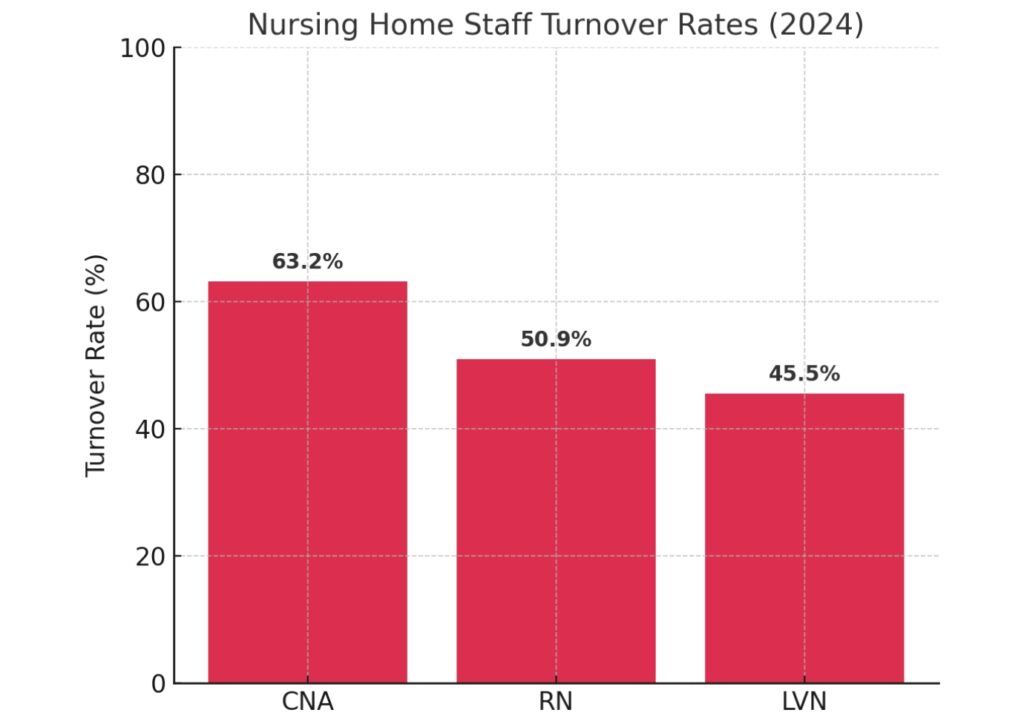
And it’s not just dollars lost. High turnover directly hurts compliance and care quality. A 10% increase in nurse turnover leads to 2.2 more deficiencies on annual surveys. That means every time a staff member walks out the door, the risk of citations—and fi nancial penalties—goes up.
The mistake many facilities make is treating staff as a cost to minimize instead of an asset to invest in. Any owner who’s been through high turnover knows—retention always pays for itself in the long run. Simple steps—like giving staff more fl exible shifts, showing them a path to grow, or just creating a workplace where people feel valued—can go a long way in cutting churn and building loyalty.
Of course, culture alone won’t fi x turnover. You also need smarter systems in place to make daily work smoother. Smarter Nurse scheduling systems reduce burnout by balancing workloads, cut down on expensive agency staffing, and ensure compliance with mandated staffing ratios.
4. Stay Ahead of Compliance & Avoid Penalties
Ask anyone in the business—few things can sink your margins faster than a compliance slip-up. One serious defi ciency can wipe out a year’s worth of profi t in a single fi ne. And yet, many
facilities still treat compliance as a back-office task instead of a frontline fi nancial strategy.
The reality: the average nursing home receives 6–7 defi ciencies per standard inspection. The most common? F880 (Infection Prevention & Control), F812 (Food Safety), F689 (Accident Hazards), F656 (Care Plans), and F761 (Drug Storage). These aren’t just clinical issues—they’re fi nancial risks.
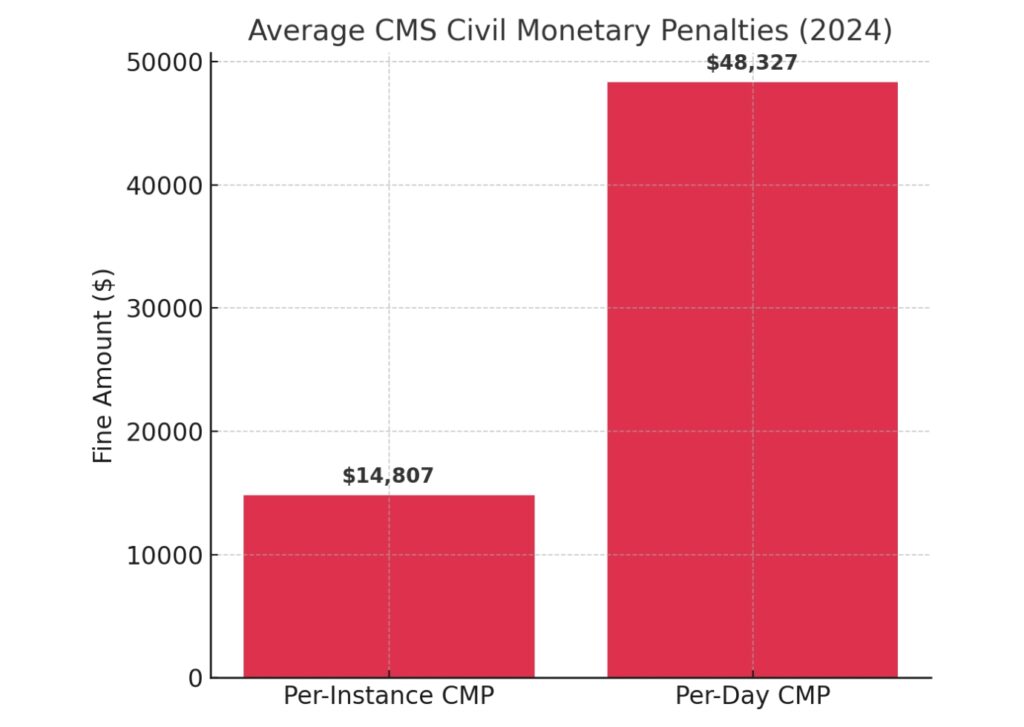
The penalties are steep. In 2024, the average per-instance Civil Monetary Penalty (CMP) was $14,807. Per-day CMPs averaged $48,327, with some cases exceeding $200,000. And if defi ciencies persist, CMS can impose a Denial of Payment for New Admissions (DPNA)—cutting off your primary revenue stream until compliance is restored.
And it’s not just about money—compliance problems also drag down your CMS star rating. That rating isn’t just a vanity metric—it directly affects referrals. Hospitals and Medicare Advantage plans fi lter facilities based on stars, which means a low score can exclude you from the most profi table referral networks.
The smarter move is to treat compliance like an investment, not just a checklist. Homes that stay proactive—training staff, monitoring daily, and keeping records ready for review—not only dodge fi nes but also earn more trust from regulators and referral partners.
5. Enhance Resident & Family Satisfaction for Growth
Profit margins don’t just come down to costs and reimbursements—they also depend heavily on your reputation. These days, a strong CMS star rating and good word-of-mouth from families matter just as much as your fi nancial reports. Families and referral partners want proof that your facility delivers quality care, and if they don’t see it, they’ll look elsewhere.
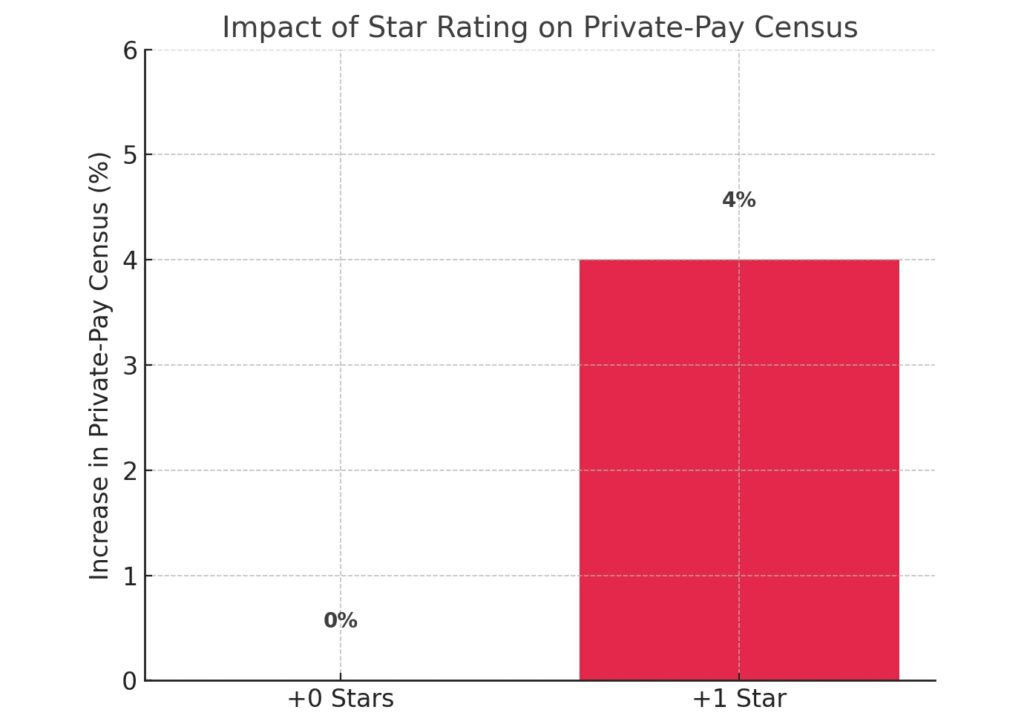
The data is clear: facilities with higher CMS star ratings consistently maintain stronger occupancy. A one-star improvement can boost private-pay census by 3–5%, which translates into hundreds of thousands of dollars in annual revenue for a 100-bed facility. That’s profi t growth without adding a single bed.
FAQs:
Let’s be real—there isn’t one simple number. Margins jump around depending on the facility. For example, the median SNF margin was about -0.3% in 2022, and almost half of facilities said they were losing money by 2024. On the other hand, the best-run nursing homes, usually the ones with a stronger payer mix and tighter systems, can pull off margins in the 8–11% range.
Some do, some don’t. If you’re heavy on Medicaid, you’re likely operating at a loss. If your census leans toward Medicare or private-pay, the numbers look much better. It really comes down to occupancy, staffing costs, and how well you run the place.
It’s usually the owners and operators who fi gure out the formula—fast admissions, fewer claim denials, stable staff, and solid compliance. It’s not about whether the home is for-profi t or nonprofi t, it’s about execution and discipline.
Around 70% of U.S. nursing homes are for-profi t. Nonprofi ts tend to put money back into staffing and care, while for-profi ts often focus more on margins. Both models have success stories, but they play the game differently.
Ethical Profitability Is Possible
Running a nursing home isn’t easy. Margins are tight, and the pressure never really stops. But profi tability doesn’t have to mean cutting staff or lowering care standards. In fact, the opposite is true.
The facilities that come out ahead are the ones that invest in people—keeping staff, building trust with families, staying ahead of compliance, and running smarter admissions. Those are the homes that manage to grow margins and deliver excellent care.
We have seen it firsthand: the operators who treat staff and residents as their strongest assets—not as expenses—are the ones who adapt and thrive.
That’s also the idea behind LTC Apps. We built it to make operations smoother, reduce waste, and keep facilities focused on what really matters—quality care and satisfi ed families.
If you’re ready to explore how your nursing home can improve margins without compromising care, let’s have that conversation.





